That Discomfort You’re Feeling Is Grief
By Scott Berinato for The Harvard Business Review
Some of the HBR edit staff met virtually the other day — a screen full of faces in a scene becoming more common everywhere. We talked about the content we’re commissioning in this harrowing time of a pandemic and how we can help people. But we also talked about how we were feeling. One colleague mentioned that what she felt was grief. Heads nodded in all the panes.
If we can name it, perhaps we can manage it. We turned to David Kessler for ideas on how to do that. Kessler is the world’s foremost expert on grief. He co-wrote with Elisabeth Kübler-Ross On Grief and Grieving: Finding the Meaning of Grief through the Five Stages of Loss. His new book adds another stage to the process, Finding Meaning: The Sixth Stage of Grief. Kessler also has worked for a decade in a three-hospital system in Los Angeles. He served on their biohazards team. His volunteer work includes being an LAPD Specialist Reserve for traumatic events as well as having served on the Red Cross’s disaster services team. He is the founder of www.grief.com, which has over 5 million visits yearly from 167 countries.
Kessler shared his thoughts on why it’s important to acknowledge the grief you may be feeling, how to manage it, and how he believes we will find meaning in it. The conversation is lightly edited for clarity.
HBR: People are feeling any number of things right now. Is it right to call some of what they’re feeling grief?
Kessler: Yes, and we’re feeling a number of different griefs. We feel the world has changed, and it has. We know this is temporary, but it doesn’t feel that way, and we realize things will be different. Just as going to the airport is forever different from how it was before 9/11, things will change and this is the point at which they changed. The loss of normalcy; the fear of economic toll; the loss of connection. This is hitting us and we’re grieving. Collectively. We are not used to this kind of collective grief in the air.
You said we’re feeling more than one kind of grief?
Yes, we’re also feeling anticipatory grief. Anticipatory grief is that feeling we get about what the future holds when we’re uncertain. Usually it centers on death. We feel it when someone gets a dire diagnosis or when we have the normal thought that we’ll lose a parent someday. Anticipatory grief is also more broadly imagined futures. There is a storm coming. There’s something bad out there. With a virus, this kind of grief is so confusing for people. Our primitive mind knows something bad is happening, but you can’t see it. This breaks our sense of safety. We’re feeling that loss of safety. I don’t think we’ve collectively lost our sense of general safety like this. Individually or as smaller groups, people have felt this. But all together, this is new. We are grieving on a micro and a macro level.
Yoga and its connection to mental health | Nikolai Blinow
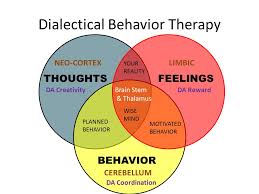
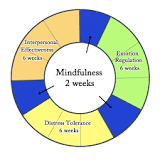
Dialectical behavior therapy (DBT)
Dialectical behavior therapy (DBT) is a type of cognitive behavioral therapy. Its main goals are to teach people how to live in the moment, cope healthily with stress, regulate emotions, and improve relationships with others.
I have been learning a lot about CBT – DBT is an interesting take on it as well.
Can You Die From Loneliness?
As a social work graduate student, I worked in a medical hospital. One of my projects included studying the “revolving door” patients — those individuals who came into the emergency room on a regular basis.
Some of these patients came into the hospital for chronic issues, such as back pain and breathing difficulties. I identified the patients who lived alone. With their permission, I began calling them on a regular basis to check on them.
Sometimes they wanted to talk about their health. At other times, they wanted to share stories about the past. I allowed them to talk about whatever they wanted and just listened.
Then, we tracked their emergency room visits. Once the calls began, their hospital visits were greatly reduced.
I think there were two reasons those phone calls reduced their visits to the hospital: they felt less lonely, which helped them feel better physically, and feeling connected with someone meant they were less likely to go to the emergency room simply to have human contact.
That was just a graduate school project with a small sample, and not exactly a peer-reviewed study. But it did give the hospital some interesting feedback about how they might be able to support some of their frequent emergency room visitors.
‘Just take a deep breath’: Why this class is learning mental health lessons
From CBC
Each student in this Winnipeg classroom has a kit full of mental health and mindfulness tools
In a middle-years classroom at Champlain School in Winnipeg, a group of students are sitting quietly on yoga mats. They’re ready for their next assignment.
At the front of the class their teacher, Catherine Siller, tells them what to do:
Anything that might be bothering us from the morning or the weekend or even from recess, I want you to focus on that energy right now. Take a deep breath in, and push that negative energy right out. – Catherine Siller
Siller is leading her Grade 5 and 6 class in a mindfulness meditation. All year long, this group of young students has been learning about the importance of caring for their mental well-being.
“What do we say?,” Siller asks as they finish the meditation.
“Namaste,” the class responds.
Building mental health toolkits
The students have been getting help throughout the school year from a cardboard box. Each student has a “Thrival Kit“, which is filled with tools to help young people work on their mental health.
Read more here, or listen to the story on CBC when you click here.
Rossy art therapy and well-being
The Michel de la Chenelière International Atelier for Education and Art Therapy makes it possible for the MMFA to consolidate its developmental focus on art therapy and well-being. All actions put in place are aimed at the same goal, namely to promote the well-being of a variety of groups, whether or not they have special needs.
In this connection, some new programming, designed in partnership with the health and academic communities, is offering a whole range of innovative projects adapted to persons living either with mental health issues, autism or eating disorders, or with difficulties related to learning, living together and social inclusion. Whether they visit exhibitions in the company of an educator, participate in creative workshops or present their creations to Museum audiences, program participants have meaningful artistic and social experiences.
Numerous professionals from the medical world and the community can join forces in an unusual practice setting, thanks to the Museum’s facilities, which include an art therapy workshop, a medical consultation room and an Art Hive, created in collaboration with the Department of Creative Arts Therapy at Concordia University.
Art has a positive effect on the physical and mental health and well-being of individuals. To back this up, researchers from various institutions in Quebec are studying the beneficial effects of a visit to the Museum, which may be comparable to the benefits of physical exercise.
Furthermore, the MMFA Art and Health Advisory Committee, composed of experts from the fields of health, art therapy, research and the arts, as well as representatives of philanthropy and the MMFA, offers its expertise and support for the development of potential partnerships and innovative projects implemented at the MMFA.
See more at the Montreal Museum of Fine Arts
3 Keys to Solving Relationship Problems
From Psychology Today
Win-win problem-solving is a matter of mastering 3 basic skills.
Disagreements, arguments are part and parcel of close relationships with partners, family, friends. While what you disagree about in a relationship is always a moving target, where most people get stuck is in 3 key areas. Here’s how to navigate them to make effective problem-solving happen:
1. Creating safety
If you feel safe in a relationship you can be honest, speak your mind, and express your thoughts and feelings and concerns without fear of the other person’s response. That doesn’t mean that the conversations at times don’t feel awkward and uncomfortable, but that from your side of it you’re not stopped by fear.
Safety is the bedrock of any close relationship. If it isn’t there what is there instead is a walking on eggshells, a shutting down, a giving in, a holding back that leads to depression or resentment or flares of anger or acting out. The lack of safety and the resulting caution can obviously come from within the relationship — that your partner has a wicked temper or is critical, that your brother is sensitive and easily feels hurt, that your friend is apt to blame you or heap on guilt. So, you don’t bring up problems with your partner for fear of the blast back, you bite your tongue with your brother because he’s not only going to feel wounded, but is likely to misunderstand your point, you water down your comment to your friend to avoid that well-known reaction.
Though your anxiety is going to tell you that safety comes only by being increasingly cautious around these folks, the path to creating a sense of safety actually comes from being bolder. You want to have a conversation about conversations, about what trigger your fears – I feel you don’t really listen and dismiss what I’m saying; you get this angry edge in your voice that makes me shut down. You do your best to be clear, and if the other person pushes back, isn’t willing to make an effort, decide what you need to do next to not feel like a victim. Don’t just take what you get.
How Addiction Affects Sleep
The quality of your sleep is affected by everything. From your habits and the food you eat, to the medications you take and drinks you ingest. So, it’s no surprise that if a person has developed an addiction—to an over-the-counter drug, alcohol, or other type of substance—that addiction could affect their sleep quality, too.
Sleep disorders and addiction have a bidirectional relationship: Each individual issue—alcohol dependence, insomnia, etc.—relate to and effect the other issue. The nature of this intricate relationship requires a person seek treatment for both issues to find a healthy, sustainable resolution.
Keep reading to discover how various forms of addiction affect sleep. This guide also will delve into various types of substance-induced sleep disorders, substances that can cause or lead to sleep disorders, and information concerning how an individual can recover from addiction.
The relationship between sleep and addiction
How do various substance addictions upset the body’s brain chemistry and disrupt the natural sleep rhythm? The answers vary. Each substance type has different characteristics, and affects an addicted person’s sleep in various ways.
Stimulants
Cocaine effects the brain’s limbic system. The system consists of interconnected regions that regulate motivation and pleasure. Cocaine’s short-term effects immediately cause a buildup of dopamine, which can cause euphoria. This euphoria can make a person want to take the drug again.
Because cocaine increases wakefulness, it can disrupt REM sleep. And cocaine withdrawal can lead to disturbed sleep and unpleasant dreams (also known as a parasomnia).
Amphetamines stimulate the central nervous system. Although amphetamines are used to treat multiple medical issues, such as depression and attention deficit hyperactivity disorder (ADHD), people can develop a psychological amphetamine dependence.
Use of amphetamines can decrease the amount of time a person spends in REM sleep periods.
Hallucinogens
Hallucinogens are a group of drugs that can alter a person’s perception, and cause sensations or create images that aren’t real. A few examples of hallucinations are as follows:
Ayahuasca
DMT
D-lysergic acid diethylamide (LSD)
Peyote (Mescaline)
4-phosphoryloxy-N,N-dimethyltryptamine (psilocybin)
In general, hallucinogens can interfere with serotonin. Serotonin regulates sleep and other major bodily functions. When a person takes a hallucinogen, they can experience short-term sleep problems. A study in the journal Therapeutic Advances in Psychopharmacology also states LSD users often experience a loss of sleep.
Sleep loss, which sometimes presentats as insomnia, can either be chronic (difficulty falling or staying asleep at least three nights a week for three months or more) or short-term (lasts less tan three months, or presents when a person has trouble falling or staying asleep).
MDMA, also known as 3,4-methylenedioxymethamphetamine or ecstasy, is a specific type hallucinogen and stimulant. It’s a synthetic drug. MDMA can make a person feel energized, and distort their perceptions and how they experience time.
People who use a lot of MDMA can experience persistent sleep disturbances. MDMA also can affect the human body’s monoamine neurotransmitters. These neurotransmitters greatly affect sleep and daytime alertness (also known as hypersomnia).
Depressants
Marijuana dependence is similar to other substance abuse disorders. People who have issues with this substance face social, psychological, and physical impairments. Dependent users also have sleep problems.
A study that appeared in the journal Sleep Medicine Reviews reports that people who smoke marijuana have a hard time falling asleep, and have strange dreams when they experience marijuana withdrawal.
Another study in the journal Addiction Science & Clinical Practice found that chronic cannabis use can negatively affect sleep during withdrawal. Insomnia, sleep withdrawal, and strange dreams were reported.
People often assume alcohol can help them sleep because it causes drowsiness. Although alcohol can help a person fall asleep, it causes disrupted sleep. Disturbances can occur during sleep stage transitions. These disturbances can worsen the effects of insomnia and cause sleep apnea.
The previously mentioned study in the journal Addiction Science & Clinical Practice also reports that alcohol users can experience:
A hard time falling asleep
Awakening during the night
Daytime sleepiness
Abnormal sleep quality
Also, insomnia is the most prevalent complaint from alcoholics after they quit drinking.
Opioids
Opioid drugs come in illegal and legal forms. Heroin, for example, is illegal, and other opioids, such as the synthetic drug fentanyl, and pain relievers, such as oxycodone, hydrocodone, codeine, and morphine, are available via prescription.
All opioids interact with opioid receptors on nerve cells in the body and brain. According to the U.S. government’s National Institute on Drug Abuse, 21 to 29 percent of patients who are prescribed opioids misuse the drugs.
Although most prescription opioids are safe to take for a short period of time, long-term opioid use can cause addiction. Addiction can occur because these pain relieving drugs also can cause euphoria.
The longer a person takes an opioid, the greater the chance they could develop an addiction. Addiction to opioids also can arise from prescription misuse.
Sadly, opioid addiction can lead to death. The CDC searchable database, CDC Wonder, reports that 20,000 overdose deaths in 2016 were related to fentanyl and synthetic opioids.
Why opioids are addictive
Environmental and individual factors impact how a person reacts to opioid drug affects. In general, however, opioids affect a person when the drug enters the bloodstream and travels to the brain.
A study in the journal Science & Practice Perspectives found that proteins that opioids attach to, which are called mu opioid receptors, are located on brain cells. This chemical/receptor interaction triggers the same biochemical brain processes that give people pleasurable feelings via “brain circuits” in the mesolimbic (midbrain) reward system.
According to the article, this “system” creates signals in the brain’s ventral tegmental area (VTA). This “area” releases the chemical dopamine (DA) in another part of the brain, which is referred to as the nucleus accumbens (NAc). Dopamine creates “pleasurable” feelings.
Opioids and sleep
Opioids are a well-known sleep disrupter. A study in the journal Anesthesiology explains that opioids can block the human body’s access to rapid eye movement (REM) sleep. These drugs also can block access to the deeper, restorative stages of non-REM sleep. A lack of sleep can actually make any pain a person may feel—for example, the pain they are taking opioids for—worse.
Opioids, withdrawal and sleep
When a person ceases using opioids, she can experience sleep issues. An article in the journal Psychiatry Research examined the quality of sleep in people who had “heroin use disorder” who were going through “early methadone maintenance therapy” (MMT). The study participants experienced less sleep and daytime sleepiness.
Another study in the journal Drug Alcohol Dependence also found that people in the early stages of methadone detox had issues getting enough sleep. Their sleep quality was poor, too.
When sleep deprivation leads to drug use
Although heavy drug use can lead to sleep issues, sleep issues, such an insomnia, can also lead to drug use.
A study published in the Journal of Youth and Adolescence found that lower levels of weekday sleep were related with substance use, specifically alcohol. An association also was found between alcohol and cigarette use and weekend oversleep, which is defined as “wake time on the weekends as compared to weekdays”. The study also posits that lower sleep times could also lower an individual’s inhibition, and their ability to regulate their emotions, which can lead to substance abuse.
Although the study examined youths’ relationship with the previously mentioned substances, the findings may relate to adults, as the study also discovered that after a follow-up, which occurred two years after the study, alcohol use was associated with weekend sleep delay (defined as a person’s time to bed on the weekends compared to weekdays). Alcohol use also was associated with greater weekend “oversleep”, too.
Important Advice for Seniors Trying to Recover Their Resilience and Joy
Growing older can be a struggle in many ways. Your body might not function the same way it used to, your income might be limited, and you just might not feel like your so-called “golden years” are so great. You might even feel depressed, anxious, or suffer from a mental health concern you don’t know how to manage. Thankfully, there are simple measures you can take to help you revive your senior years and recover your joy.
You Aren’t Alone
Does it feel like you’re stressed out, worn out, weary, or just can’t find happiness? Many people have mental wellness concerns, and just because you make it to your senior years doesn’t mean there won’t be bumps in the road. In fact, studies cited by US News indicate that up to 20 percent of older adults struggle with mental health. Diagnosis can be challenging since many seniors take medications that can cause or imitate symptoms of issues such as depression.
Recognizing Trouble
Issues such as depression can be an elusive concern for seniors since so many other troubles can look similar to depression. For instance, many people attribute a loss of interest in activities, inability to sleep, reduced appetite, and insomnia with the aging process, but those problems can relate to depression. Seniors can feel moody, confused, or experience memory loss due to depression as well, and oftentimes others might think it’s “just old age.” There are also medications for certain chronic conditions that could contribute to those concerns, so doctors and family members might overlook the signs you are feeling depressed.
Taking Action
One simple way to combat mental wellness concerns is to declutter your home. Clutter appears to be linked to depression, anxiety, and stress, and tidying up can make you feel better about yourself and your home. If it’s too overwhelming or you don’t have time to undertake the endeavour yourself, consider investing in having a professional do it on your behalf. Most homeowners spend between $100 and $200 for thorough routine house cleanings. Another suggestion is to engage in some healthful activities, such as getting involved with a group that shares your interests. You can join a book club, play cards or dominoes, or volunteer at a local charity. Ensure you’re eating a nutritious diet, and spend some time outdoors every day.
Managing Trauma
Did something traumatic occur in your life, and you’re trying to manage in spite of it? You might feel like you can “get over it,” especially since you already have many experiences to draw from. However, according to some studies, many seniors struggle with PTSD, and it can stem from an old stress newly surfacing, or from a new traumatic incident. Symptoms include things like insomnia, moodiness, and social withdrawal. There are many methods for managing PTSD symptoms, such as through meditation, exercise, and aromatherapy. Psychiatric Times notes that seniors often worry about what others might think if they seek treatment for their symptoms of mental health concerns such as PTSD, but it’s vital to get help if you need it, and nobody needs to know except you and your counselor or doctor.
Connecting with Help
Many people need help at some point in life, and it’s no shame to reach out when you need assistance. In fact, some research reflects that seniors are at the biggest risk for suicide. If you are using medications beyond prescribed dosages to manage pain, thinking about hurting yourself, experiencing lethargy, or just don’t feel good, you don’t need to suffer. You can talk with your physician, or there are several free, confidential hotlines you can call for assistance.
- National Suicide Prevention Lifeline: 1-800-273-8255
- Substance Abuse and Mental Health Services Administration: 1-800-662-4357
- National Hopeline Network: 1-800-SUICIDE (784-2433)
It’s important to be aware of the symptoms you’re experiencing. If you are feeling down, edgy, worn or weary, it doesn’t have to be that way. You can rediscover your joy and resilience, just reach out for help — and don’t feel ashamed to do so.
Image courtesy of Pixabay