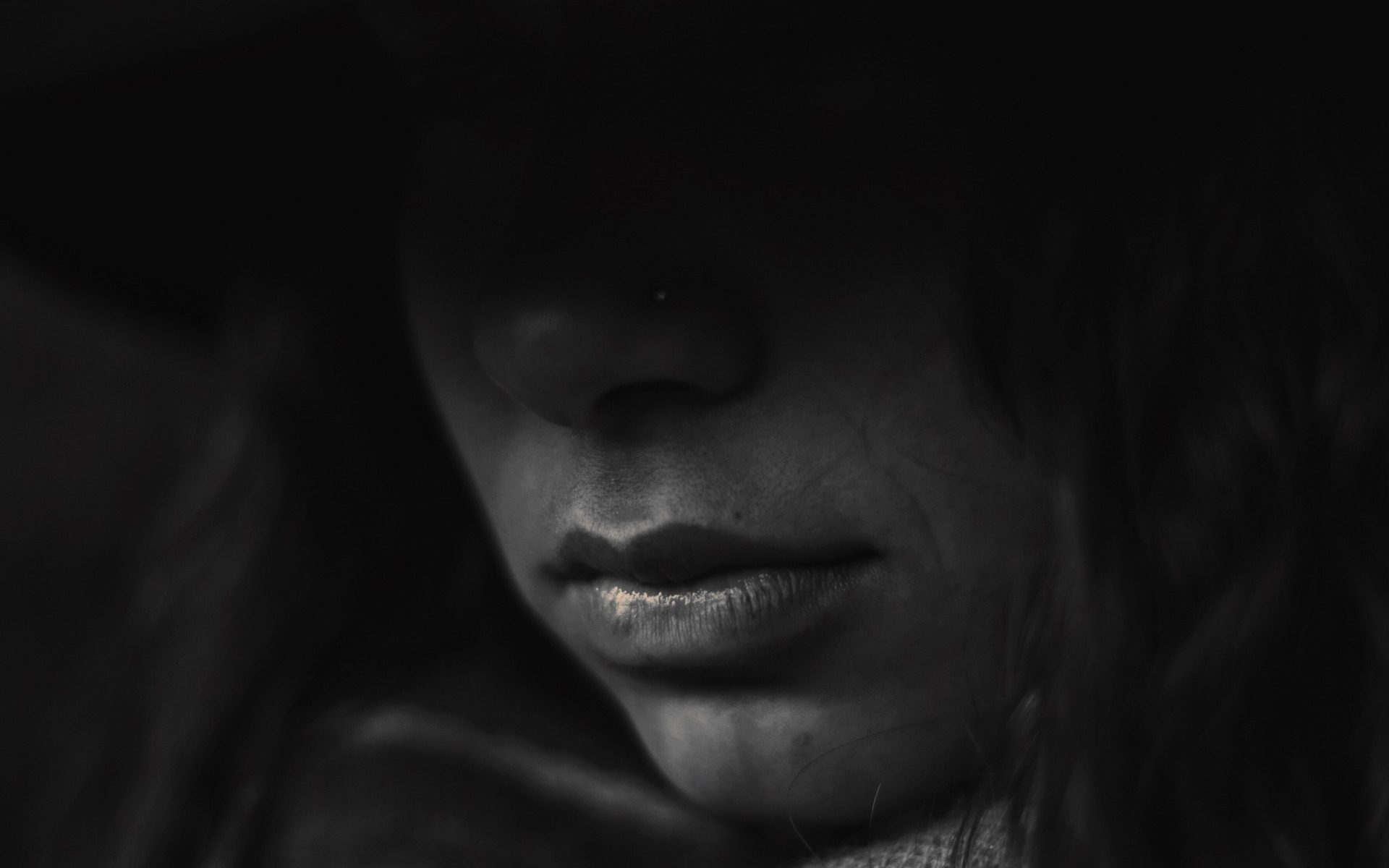
Outbreaks can be stressful
The outbreak of coronavirus disease 2019 (COVID-19) may be stressful for people. Fear and anxiety about a disease can be overwhelming and cause strong emotions in adults and children. Coping with stress will make you, the people you care about, and your community stronger.
Stress during an infectious disease outbreak can include
- Fear and worry about your own health and the health of your loved ones
- Changes in sleep or eating patterns
- Difficulty sleeping or concentrating
- Worsening of chronic health problems
- Worsening of mental health conditions
- Increased use of alcohol, tobacco, or other drugs
Everyone reacts differently to stressful situations
How you respond to the outbreak can depend on your background, the things that make you different from other people, and the community you live in.
People who may respond more strongly to the stress of a crisis include
- Older people and people with chronic diseases who are at higher risk for severe illness from COVID-19
- Children and teens
- People who are helping with the response to COVID-19, like doctors, other health care providers, and first responders
- People who have mental health conditions including problems with substance use
Take care of yourself and your community
Taking care of yourself, your friends, and your family can help you cope with stress. Helping others cope with their stress can also make your community stronger.
Ways to cope with stress
- Take breaks from watching, reading, or listening to news stories, including social media. Hearing about the pandemic repeatedly can be upsetting.
- Take care of your body.
- Take deep breaths, stretch, or meditateexternal icon.
- Try to eat healthy, well-balanced meals.
- Exercise regularly, get plenty of sleep.
- Avoid alcohol and drugsexternal icon.
- Make time to unwind. Try to do some other activities you enjoy.
- Connect with others. Talk with people you trust about your concerns and how you are feeling.